November 2025 Board of Health Meeting - 2026 Annual Service Plan Auxiliary Report
Background
The Windsor-Essex County Health Unit (WECHU) is a publicly funded organization; as such the WECHU has a responsibility to spend funds prudently with the objective of providing public health programs and services as required by the Health Protection and Promotion Act (HPPA) and the Ontario Public Health Standards: Requirements for Programs, Services, and Accountability (OPHS).
The WECHU receives funding in the following manner:
- The Ministry of Health (MOH) grants the WECHU annual funding to a maximum of 75% of admissible expenditures for local health protection and promotion programs, with the Corporation of the City of Windsor, the Corporation of the County of Essex, and the Corporation of the Township of Pelee (hereinafter collectively referred to as the “Obligated Municipalities”) required to contribute a minimum of 25% of admissible expenditures.
- The Province of Ontario has committed to providing local public health units with an annual one per cent funding increase through 2026.
- In addition to base funding, historically the Ministry of Health (MOH) annually provides grants and one-time funding for programs that address emerging areas at a rate of 100% of admissible expenditures. Although limited in comparison to previous years, submissions for one-time funding costs in 2025 into the first quarter of 2026 included requests to support funding for Measles and Respiratory Syncytial Virus Vaccine.
- The Province of Ontario, more specifically the Ministry of Children, Community and Social Services (MCCSS), provides annual grants to fund the Healthy Babies Healthy Children Program Initiative at a rate of 100% of admissible expenditures. A funding increase was provided in 2025 to support program operations.
On an annual basis, the WECHU prepares its operating budgets for review and approval by the Board of Health (BOH). The budget then becomes the foundation for the Annual Service Plan and Budget Submissions to the MOH and MCCSS. Quarterly, a budget-to-actual variance analysis is prepared for the BOH to supplement the quarterly reporting requirements to both the MOH and MCCSS.
Community Needs and Ministry Requirements
To understand our planned services and budget, it is important to first consider the needs of the Windsor and Essex County (WEC) community, including the public health challenges we aim to address with limited financial and human resources. Population health assessment and surveillance activities provide the evidence base for determining community priorities, identifying health inequities, and aligning local efforts with provincial requirements established through the Ontario Public Health Standards (OPHS) and related legislation.
Since the completion of Community Needs Assessments (CNA) in 2016 and 2019, the WECHU has continued to enhance its capacity for surveillance and analysis of population health trends through the development and maintenance of interactive, publicly available data dashboards. These dashboards provide current local information on oral health, infectious diseases, immunizations, chronic diseases, reproductive and child health, injury, substance use, and mental health, supporting transparency, data-informed planning, and community awareness of local health issues.
Population health assessment remains a central component of the WECHU’s annual priority-setting and budget development processes. Since 2023, the WECHU has conducted an annual, structured program review requiring each program area to assess and present evidence on the size and severity of health issues, existing community coverage, related health inequities, and the effectiveness of local interventions. Findings from the 2025 review directly informed 2026 service planning and resource allocation, ensuring that programming decisions are evidence-based and responsive to emerging community needs.
Local Priority Populations
Priority populations are a subset of the population for whom a specific program is tailored based on marginalization, vulnerability, or other risk factors. The Ontario Public Health Standards (OPHS) mandate boards of health to identify local priority populations at increased risk of poor health outcomes and plan and deliver programs and services to reduce these inequities. Local data illustrate the extent of these inequities and help identify the populations most affected.
In WEC, disparities persist related to income and food security. The proportion of individuals living in low-income households remains higher across nearly all age groups compared to Ontario, with 16.5% of children aged 0–5 and 14.5% of children under 18 living below the low-income measure after tax (LIM-AT), compared to 12.4% and 11.5% provincially. One-quarter of children (25.7%) live in single-parent households, and food insecurity affects nearly one in five households (18.9%), up from 17.4% in 2019–2020.
The region is also home to the largest population of International Agricultural Workers (IAWs) in Canada, with approximately 8,000–10,000 workers employed each year. WEC’s population is increasingly diverse, with 24% identifying as visible minorities and 23% identifying as immigrants, including 4% who are recent newcomers from Iraq, Syria, and India.
According to a recent research study conducted by the WECHU in 2024-2025, one in three low socioeconomic status (SES) residents rate their overall health as only fair or poor, nearly double the rate among higher-income residents. Low SES residents were more than twice as likely to report running out of food with no money to buy more, and many cited financial stress, affordability, limited access to healthy food and physical activity opportunities as major barriers to staying healthy.
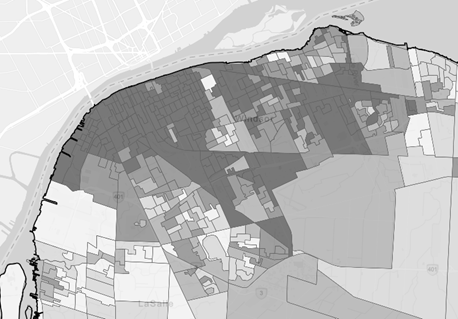
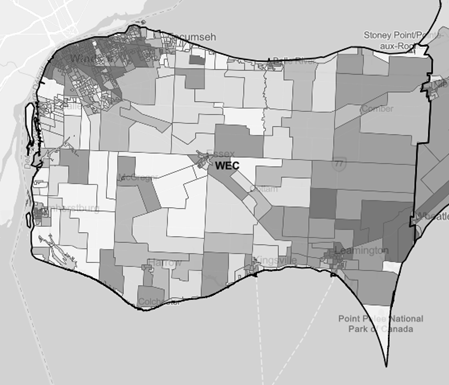
To better understand and address these inequities, the WECHU has begun using the Ontario Marginalization Index (ON-Marg) as a tool for identifying and targeting priority populations. The WECHU specifically applies the Material Resources dimension of the index, which measures access to basic material and financial resources such as income, employment, and education. Within this framework, the WECHU focuses on residents living in quintile five (those experiencing the highest level of material deprivation). The maps below provide a visual overview of areas in Windsor and Essex County with the highest levels of material deprivation.
Unique Local Challenges and Risks
The WECHU catchment area shares a border with Detroit, Michigan, which is the busiest international border crossing in North America. This border contributes to public health areas of concern including transmission of communicable diseases, as well as known zoonotic disease vectors (e.g., exotic mosquito species). Monitoring and surveillance of these public health concerns in Michigan is required, as many individuals in WEC visit or work in Michigan daily. More recently, political polarization has created barriers for cohesive public health surveillance and assessment, and the potential economic impact of proposed tariffs would cause further instabilities, which in turn negatively affect community health and well-being. As of September 2025, WEC has an unemployment rate of 10.4%, which is the highest rate in Canada.
The leading causes of preventable deaths in WEC as of 2022 were cancer, circulatory system diseases, and respiratory system diseases, all of which exceed provincial rates. Rates of all-cause mortality, premature mortality, and potentially avoidable mortality also remain higher in WEC compared to Ontario. Education and employment patterns further influence local health outcomes. In 2021, 51% of adults in WEC had post-secondary education, 32% held a high school diploma, and 18% had less than a high school education. Overall, educational attainment in WEC is lower than Ontario. The most common industry in WEC is manufacturing which accounted for 20% of the labour force (this is 2.1-times greater than the equivalent Ontario value). In 2020, 21% of the population aged 15 years and over in WEC, received their income from government transfers.
Access to primary care remains an ongoing challenge, particularly for low-income residents. In 2024, thirteen percent of Windsor-Essex residents report not having a family doctor, and nearly one in three (31%) residents in the lowest income bracket do not have a regular healthcare provider, compared to only 5% among those in the highest income bracket.
Opioid-related Emergency Department (ED) visits increased sharply from 10.06 visits per 100,000 population in 2015 to 95.93 in 2024, remaining higher than provincial rates for most years since 2015. Cocaine-related ED visits reached 90.75 per 100,000 in 2024, exceeding Ontario’s rate (77.96 per 100,000), and alcohol-related hospitalizations were higher in WEC (271.78 per 100,000) than provincially (192.77 per 100,000).
Infectious diseases continue to present significant local challenges. A measles resurgence in early 2025 resulted in 150 reported cases, while the rate of influenza increased by 231% between 2023 and 2024, rising even further by mid-2025. Sexually transmitted and blood-borne infections (STBBIs) are also increasing, with the syphilis rate rising from 17 per 100,000 in 2023 to 21 per 100,000 in 2024, including three congenital syphilis cases. Active tuberculosis (TB) cases increased from 10 in 2023 to 17 in 2024, alongside 287 cases of latent TB.
Vector-borne and zoonotic disease surveillance identified eight mosquito pools positive for West Nile Virus in 2024, resulting in seven human cases. Seventeen Lyme disease cases were reported in 2024, with four additional cases in the first half of 2025.
Environmental health and seasonal housing also present unique local considerations. The WECHU inspects approximately 1,200 seasonal housing accommodations every eight months, as required by the Government of Canada. WEC has the largest population of International Agricultural Workers (IAWs) in Canada, with 8,000–10,000 workers employed annually.
There were seven public beaches monitored weekly in 2025 for E. coli from June to September. During the season there were 25 water-quality warnings and five closures issued
Pelee Island, accessible only by air or water, contains most of the region’s 34 Small Drinking Water Systems (SDWS). The island’s remoteness creates operational challenges for inspections, particularly during off-season months.
Windsor and Essex County are also located within the primary and secondary zones of two nuclear installations (Enrico Fermi 2 and the Davis-Besse). Although both installations are not located within Canadian borders, the impact they have on our region is the same in the event a nuclear emergency occurs. According to the Canadian Nuclear Safety Commission (CNSC), all nuclear installations must ensure that KI tablets are pre-distributed, and that pre-distribution includes a public education plan. Since the Enrico Fermi 2 Nuclear Generating Station and the Davis – Basse Nuclear Power Station are not regulated by the CNSC, the responsibility for KI tablet distribution falls on the WECHU, the Municipalities of WEC, and the Ministry of Health.
Program Standards
The WECHU’s programs and services are informed by the Program Standards outlined in the new 2026 Ontario Public Health Standards (OPHS), which articulate the ministry’s expectations for boards of health and outline the minimum requirements for public health programs and services (with the exception of pending protocols and one program standard). The new OPHS, which come into effect in January 2026, defines the mandate of boards of health and provide a framework for planning, service delivery, and budget development. Within this framework, programs are tailored to the local context.
Comprehensive Health Promotion
The goal of the Comprehensive Health Promotion standard is to enable individuals, families, and communities to achieve their full health potential by fostering healthy social, natural, and built environments. Under this standard, boards of health are required to use coordinated, evidence-informed strategies to address the determinants of health and promote well-being across the life course.
Among young children, one in four kindergarten students (28.1%) were vulnerable in at least one developmental domain in 2017–2018, an increase from 24.9% in 2013–2014. Vulnerability in language and cognitive development (9%) was higher than the provincial rate (7.5%).
Access to food is an increasing challenge in WEC. Between 2023 and 2024, 25.7% of people in Windsor-Essex were living in a food-insecure household. Further, in 2023, 12.9% of children 1 to 17 years old in WEC live in food-insecure households.
In 2023, 16.6% of students reported struggling with their mental or emotional health, while 23% of students in grades 9 to 12 felt depressed most days in the past week and 37% felt anxious or on edge. Rates of poor self-reported mental health were highest among females (26.1%) and 2SLGBTQIA+ youth (61.6% by gender identity, 41.4% by sexual orientation). 14.7% percent of WEC students considered attempting suicide, and 5.3% reported a previous attempt.
The 2020 Canadian Community Health Survey (CCHS) data for Windsor-Essex County reported that 19.3% of respondents had experienced at least one childhood maltreatment incident. Although ACES are common, there are significant disparities across populations. A recent study revealed higher prevalence of more ACES among certain groups, including Indigenous people (40.8%), low-income households (40.5%), the unhoused (59.7%), individuals with mental health conditions (47.5%) or substance use issues (55.2%), and those with a history of criminality (31.8%) (Madigan, 2023).
Nearly one in five adults (19.3%) reported at least one form of childhood maltreatment, and intimate partner violence continues to be a major public health issue. In 2024, 30% of all crimes against persons in Windsor were related to intimate partner violence, resulting in more than 2,500 police calls between January and August.
Finally, oral health surveillance continues to demonstrate that children from schools associated with lower socioeconomic status had the worst oral health outcomes locally (e.g., prevalence of caries). In 2023, there was 142% increase in the percentage of children with urgent dental needs, such as large lesions, infection, trauma, or irreversible periodontal disease. Demand for the Ontario Seniors Dental Care Program (OSDCP) remains high, with 2,386 OSDCP cards issued and 1,082 seniors receiving treatment through WECHU clinics between August 2024 and April 2025.
Below is a list of the program(s) under the Comprehensive Health Promotion standard along with examples of work included under each.
Healthy Pregnancy and Preparation for Parenting Education
- Offering healthy pregnancy and preparation for parenting and breastfeeding focused classes in WEC, including Building Blocks for Better Babies in partnership with the University of Windsor.
- Engaging with local health professionals and community partners to provide evidence-based resources, and appropriate referrals to Healthy Babies Healthy Children program and other community agencies.
- Collaborating with community partners to develop a comprehensive perinatal, infant, and early childhood mental health pathway.
Healthy Growth and Development
- Implementing interventions that address communicable disease (e.g., promote vaccination) and non-communicable disease prevention (e.g., physical activity, sleep).
- Collaborating with high-risk childcare and school partners to monitor high absenteeism.
- Engaging with families to understand the root causes of student (school based) absenteeism and create strategies to address these issues.
- Providing evidence-informed health and wellness resources and training to early childhood educators and families.
- Assessing, advocating and co-planning interventions for policy implementation using Community Health Action Plans (CHAPS) that improve health and reduce health disparities resulting from barriers to the social and structural determinants of health.
The Healthy Babies and Healthy Children Program (funded by MCCYS)
- Collaborating with community partners to promote the Healthy Babies Healthy Children Program.
- Providing home visits to families identified with risk to enhance prenatal, postpartum, and parental support, and enhance infant and early childhood development.
Food Environment
- Implementing a food insecurity screening and referral system with community partners.
- Promoting and supporting the initiation and continuation of breastfeeding from birth to up to 2 years and beyond.
- Initiating an infant feeding surveillance survey to capture detailed, local data about infant feeding in Windsor and Essex County.
- Working with schools and childcare providers to deliver education about food literacy, food skills, food neutrality, and weight-inclusivity to families with young children and youth (age 0-18).
- Working with strategic partners on school-based food programs.
- Working with the Food Policy Council to identify where local or regional policies can be updated or created that will decrease food insecurity and reduce health inequities that impact our most vulnerable population’s access to food.
Healthy Relationships
- Supporting early relational health by providing evidence-based resources on the importance of healthy relationship building and its connection to mental health and healthy growth and development.
- Working interdepartmentally and with community partners on interventions that address the impact that Positive and Adverse Childhood Experiences (PACEs) have on the most vulnerable populations.
- Working with the public-school board to support sexual health education by providing resource support on topics such as gender identity and expression, and gender-based violence.
- As part of a PHAC grant and in partnership with the University of Windsor, working with school boards to deliver the “Flip the Script with E-AAA™ program to local high needs schools, targeting students who are female or who identify as female.
- Implementing youth relationship violence initiatives with the WECHU-led Youth Relationship Violence Prevention Community of Practice (COP) which is supported by organizations who have a vested interest in youth relationship violence prevention specifically for young women and individuals who identify as 2SLGBTQINA+.
Mental Health Promotion
- Engaging with school boards and high priority schools to co-plan evidence-based interventions (School Assessment Survey and School Health Action Plans [SHAPS]) and inform policies that encourage positive mental health and well-being while creating inclusive and welcoming environments for all students.
- Engaging with educators in high needs schools to implement tier-one level programs focusing on mental health promotion/social emotional skills and resilience building, and implementing education programs that address stigma, discrimination, and improve social inclusion.
- Creating and promoting resources with community partners and school boards that increases digital media literacy and addresses the prevention and reduction of problematic technology use.
- Identifying and informing policies that reduce barriers and inequities that impact our most vulnerable population’s access to mental health supports (e.g., PPM 128).
- Facilitating the WECHU 2SLGBTQIA+ Youth Advisory Committee to improve equitable access to services and supports, inclusivity, and acceptance of 2SLGBTQIA+ youth in the community and various settings through policy development and initiatives.
Healthy Smiles Ontario
- Operating two fixed dental clinics that offer direct clinical services to Healthy Smiles Ontario (HSO) clients including preventative and emergency services.
- Connecting clients to community dental offices and covering the fees for service for those eligible.
- Supporting families with children and youth 17 years of age and under to improve their oral health knowledge and awareness of oral health services through targeted outreach to priority populations.
- Providing support for enrollment in the Canadian Dental Care Plan to ensure the most accessible service is available to clients.
Ontario Seniors Dental Care Program
- Operating two fixed dental clinics that offer clinical service delivery to OSDCP clients including preventative and emergency services.
- Connecting clients to community dental offices and covering the fees for service for those eligible in order to reduce wait times and better access to care.
- Providing support for enrollment in the Canadian Dental Care Plan to ensure the most accessible service is available to clients.
- Assisting eligible seniors 65 years old and older to enroll in the OSDCP, including support to complete and submit the required documentation and consents.
Oral Health Assessment and Surveillance
- Providing oral health screenings of Grade JK, SK, 2, 4, and 7 students (based on school risk assessment) in elementary schools annually by registered dental hygienists to identify children in need of dental care.
- Notifying parents of all children who are screened and identified in need of preventive and/or essential oral health services, enrolling eligible children in the Healthy Smiles Ontario program, and helping parents/guardians that may face language barriers.
- Ensuring timely treatment occurs for those children who screen with dental issues by working with community dental offices and Children’s Aid Services.
- Conducting a needs assessment to determine the value of integrating visual health screening into oral health screening protocols for high needs schools in future years.
- Developing a Visual Health Information Sheet for distribution alongside school oral health screening materials.
Food Safety
Under the Food Safety Standard, boards of health are required to prevent or reduce the burden of foodborne illness in the community.
Currently, the WECHU inspects 3058 fixed food premises annually. Of these, 456 are categorized as high-risk food premises and 1427 moderate-risk food premises. These include institutional facilities, restaurants/take out service, home-based and rental kitchens. Additionally, 219 temporary transient facilities were inspected from January to September 2025.
Between January and July 2025, WECHU received 177 food safety complaints that prompted investigations and/or inspections. During this time, one Provincial Offences ticket was issued for the absence of a certified food handler on site, and six Section 13 orders were issued in response to pest infestations, lack of hot water, and unsanitary conditions.
To strengthen food safety knowledge and promote compliance, WECHU issued 1,470 food handler certificates in 2024 through 59 public and 5 private exam sessions.
In 2024, 248 cases of reportable enteric diseases were identified in Windsor and Essex County. Between January and July 2025, 103 cases reported. In both 2024 and 2025, Campylobacter Enteritis and Salmonellosis were the most common enteric diseases.
Below is a list of the program(s) under the Food Safety standard along with examples of work included under each.
Food Safety Program
- Conducting routine inspections based on risk level and re-inspections of food premises, including those that cater to the seasonal worker population, local special events, and seasonal premises.
- Receiving and investigating all public complaints related to food premises including uninspected homebased food businesses.
- Operating a 24/7 on-call system for receiving and responding to food-borne illnesses/outbreaks or regulation non-compliance. This also includes emergency response to floods, fires, power outages, or other situations that may affect food safety.
- Maintaining the Food Safety Inspection Dashboard, and the disclosure website to share inspection outcomes, including those from approved home-based businesses.
- Providing food safety awareness, education, training, and certification which includes operating the local Food Handler Certification Program.
Health Hazard Management
The goal of the Health Hazard Management standard is to reduce exposure to health hazards and mitigate existing and emerging risks.
Recent environmental and local surveillance data continue to guide WECHU’s health hazard management activities. Trends reported by Environment and Climate Change Canada indicate that the Windsor-Essex region has experienced some of the warmest years on record within the past 25 years, with mean temperatures in the City of Windsor rising by approximately 1°C between the 1960–1989 and 1990–2019 periods. The median number of days with temperatures above 30°C is projected to increase from about 22 days per year (2005–2017) to nearly 50 days per year by the 2040s (City of Windsor, 2020). In response, the WECHU issued four heat warning notifications in 2024, covering 14 days, and an additional six heat alerts between January and July 2025, spanning approximately 18 days.
Air quality also remains a concern due to Windsor’s proximity to major industrial areas and its location along one of North America’s busiest trade corridors. In 2024, Air Quality Ontario recorded 59 days in downtown Windsor and 65 days in Windsor West where the Air Quality Health Index (AQHI) reached a moderate or higher risk level, a slight improvement compared to 2023 but still indicative of ongoing exposure risks for vulnerable populations.
Occupational and residential hazards associated with agriculture and agribusiness also represent a significant area of local public health action. WEC has the largest agricultural industry in Ontario, employing an estimated 8,000 to 10,000 International Agricultural Workers (IAWs) annually, primarily from Mexico and Jamaica. In 2024, WECHU conducted 1,034 compliance inspections and 251 re-inspections for seasonal housing accommodations, ensuring that workers living environments met health and safety standards.
Below is a list of the program(s) under the Health Hazard Management standard along with examples of work included under each.
Health Hazard Management
- Providing direction on the investigation, assessment, and management of mitigation strategies for all emerging hazards.
- Inspecting and providing education to all recreational camps, ice rinks/arenas, seasonal farm worker housing and special care homes for potential health hazards.
- Inspecting schools, licensed childcare centres, shelters, and other facilities that may serve priority populations when there is an identified health hazard.
- Conducting complaint-based inspections at food establishments and tanning salons to ensure compliance with the Menu Labelling Protocol, and Tanning Beds protocol respectively.
- Providing timely response and information to potential and confirmed hazardous environmental exposures, including biologic agents and other emerging environmental exposures. This includes the distribution of Potassium Iodide (KI) pills to residents in high-risk zones as a part of nuclear emergency preparedness programming.
Immunization
The goal of the immunization standard is to reduce or eliminate the burden of vaccine-preventable diseases through immunization.
Measles activity increased significantly in WEC in early 2025, with 147 confirmed cases between January and June, representing a rate of 29 cases per 100,000 population. This puts WEC among the hardest-hit regions by the provincial outbreak of measles. Measles vaccine coverage among 7-year-olds was 88.68%, below the national target of 95%, though gradually improving from 83% in 2020–2021. Coverage rates among 12-year-olds (92.49%) and 17-year-olds (93.25%) were higher but still short of national goals.
The rate of laboratory-confirmed influenza increased by 231%, from 42 cases per 100,000 in 2023 to 139 per 100,000 in 2024 and reached 214 per 100,000 between January and June 2025. During the 2024–2025 season, 79,140 influenza vaccine doses were distributed locally. Vaccination coverage among long-term care residents was 89.3%, exceeding the provincial rate (88.3%), and 69.5% were vaccinated against RSV, below Ontario’s rate of 73.1%.
The burden of COVID-19 in WEC has decreased, though deaths and outbreaks continue to occur. In 2024, there were 40 local COVID-19 deaths and 107 outbreaks investigated; between January and June 2025, 10 deaths and 13 outbreaks were reported, with 203 residents hospitalized. Vaccine uptake has declined considerably, with only 9.8% of residents receiving a Fall 2024–2025 COVID-19 booster. As of March 2025, just 1% of those under 18 and 34.5% of seniors (65+) were up to date with COVID-19 vaccination. Between January and June 2025, the Mobile Medical Support (MMS) team operated 7 mobile clinics and 71 in-house clinics, administering 401 COVID-19, 172 influenza, and 61 RSV vaccines to high-priority populations.
Between January and June 2025, WECHU fulfilled 1,913 vaccine orders, distributing over 120,000 doses of publicly funded vaccines to local healthcare providers. During the same period, 21 adverse events following immunization (AEFIs) were reported, including one following COVID-19 vaccination.
Among 7-year-olds in 2024–2025, vaccine coverage for diphtheria (88.22%), measles (88.68%), mumps (88.44%), pertussis (88.16%), polio (88.14%), rubella (93.3%), tetanus (89.04%), and varicella (87.6%), was below the national goal of 95% by age 7. Coverage among 12-year-olds was higher: diphtheria (92.22%), measles (92.49%), mumps (92.37%), pertussis (92.14%), polio (92.37%), rubella (93.29%), tetanus (92.31%), varicella (91.3%), and meningococcal disease (84.22%). For 17-year-olds, rates were higher: diphtheria (90.57%), measles (93.25%), mumps (93.19%), pertussis (90.7%), polio (93.11%), rubella (94.74%), tetanus (90.61%), varicella (%), and meningococcal disease (93.99%). Vaccination rates among 17-year-olds have improved compared to previous years, with most now meeting the 90% national coverage target.
Below is a list of the program(s) under the immunization standard along with examples of work included under each.
ISPA Implementation in Schools and Licensed Childcare Settings
- Assessing the immunization records of students in schools to determine coverage rates and enforce the requirements of the Immunization of School Pupils Act (ISPA).
- Conducting informational campaigns to educate parents, school and childcare setting administrators, and healthcare providers about the ISPA requirements and role the WECHU plays in implementation.
Vaccine Administration
- Providing school-based and on-site immunization clinics to eligible grade 7 students.
- Providing immunizations to highest risk groups, as mandated by the Ministry of Health, of publicly funded vaccines.
- Providing immunization clinic assistance in the event of an outbreak or occurrence of a Disease of Public Health Significance (DoPHS) requiring post-exposure prophylaxis.
Vaccine Confidence
- Assessing and gaining insights on local vaccine confidence rates to identify key groups and/or areas of focus.
- Implementing evidence-informed strategies aiming at increasing confidence in vaccination and immunization as a preventive strategy.
Vaccine Management
- Managing the supply and distribution of publicly funded vaccines to local health care providers to support equitable allocation based on need.
- Enhancing vaccine ordering and inventory management systems to improve efficiency and accuracy.
- Promoting, monitoring, and enforcing effective vaccine inventory management to limit vaccine waste and promote vaccine safety.
- Conducting annual vaccine refrigerator inspections for all health care providers who store publicly funded vaccines to ensure adherence to cold chain requirements.
COVID-19 Vaccine Program
- Offering COVID-19 vaccines based on Ministry of Health guidance for high risk and vulnerable populations through on-site clinics and/or mobile clinics.
- Managing supply and distribution of COVID-19 vaccines to local healthcare providers.
- Monitoring and enforcing vaccine inventory management for all Windsor-Essex County providers administering COVID-19 vaccine in accordance with reconciliation requirements from the ministry.
RSV Vaccine Program
- Offering RSV vaccines based on Ministry of Health guidance for high-risk and vulnerable populations through on-site clinics and/or mobile clinics.
- Managing the supply and distribution of RSV vaccines to local healthcare providers.
- Monitoring and enforcing vaccine inventory management for all Windsor-Essex County providers administering RSV vaccines.
Infectious and Communicable Diseases Prevention and Control
The goal of the Infectious and Communicable Diseases Prevention and Control standard is to reduce the burden of communicable diseases and other infectious diseases of public health significance.
Local surveillance data highlight ongoing activity across multiple disease categories. Excluding COVID-19, the greatest disease burden in 2024 was from sexually transmitted and blood-borne infections (STBBIs), followed by respiratory and enteric diseases. In the first half of 2025, influenza became the leading cause of infectious disease, followed by STBBIs, measles, and latent tuberculosis. The WECHU investigated and managed 183 outbreaks in 2024 and 90 outbreaks between January and June 2025 (52 respiratory, 36 enteric, and 2 other pathogens).
Among STBBIs, infectious syphilis increased by 24%, from 17 to 21 cases per 100,000 between 2023 and 2024, with three congenital cases reported in 2024. From January 1 to June 30, 2025, the rate of infectious syphilis in WEC was 10 cases/100,000 population and there were 3 cases of congenital syphilis. The rate of HIV cases in WEC decreased by approximately 17% from 12 cases/100,000 population in 2023 to 10 cases/100,000 population in 2024. From January 1 to June 30, 2025, the rate of HIV in WEC was 2 cases/100,000 population. The rate of chlamydial infections in WEC decreased by approximately 5% from 177 cases/100,000 population in 2023 to 168 cases/100,000 population in 2024. From January 1 to June 30, 2025, the rate of chlamydial infections in WEC was 67 cases/100,000 population.
Tuberculosis (TB) remains an ongoing focus of prevention and treatment. There were 10 active TB cases (2 per 100,000) and 325 latent TB cases (70 per 100,000) in 2023. In 2024, active TB rose to 17 cases (4 per 100,000), while latent TB declined slightly to 287 cases (58 per 100,000). Between January and June 2025, 11 active TB cases (2 per 100,000) and 140 latent TB cases (28 per 100,000) were reported.
Vector-borne and zoonotic diseases continue to be monitored through ongoing surveillance. In 2024, eight mosquito pools tested positive for West Nile Virus (WNV), and seven human cases were identified. None have been detected to date in 2025. Seventeen human cases of Lyme disease were reported in 2024, and four in 2025, with no blacklegged ticks collected locally during 2024 or 2025 surveillance. Animal exposure investigations remain frequent with 1,044 cases reviewed in 2024, and 520 cases between January and June 2025.
Below is a list of the program(s) under the Infectious and Communicable Diseases Prevention and Control standard along with examples of work included under each:
Facility Infection Prevention Compliance
- Conducting routine inspections of all long-term care homes, retirement and rest homes, correctional facilities, licensed childcare centres, and personal service settings for adherence to Infection Prevention and Control (IPAC) practices.
- Conducting inspections and providing education at both routinely inspected premises (e.g., long-term care homes) and non-routinely inspected premises (e.g., group homes) in the event of an outbreak.
- Facilitating an online course for personal service setting operators and staff to assist in meeting their legislated training requirements.
- Providing public disclosure of all confirmed IPAC lapse investigations for personal service settings, childcare settings, regulated health care facilities, unlicensed childcare settings, community centres, recreational facilities, schools, and temporary dwellings for seasonal workers.
Zoonotic and Vector-Borne Disease Management
- Supporting seasonal surveillance of ticks and mosquitoes, as well as ongoing prevention of human cases of rabies, Lyme disease, West Nile Virus, Eastern Equine Encephalitis (EEE), Zika, and emerging vector borne diseases in our region.
- Following up within 24 hours on all confirmed cases of avian chlamydiosis, avian influenza, novel influenza, and echinococcus multiocularis in mammals or other emerging Vector-Born Diseases (VBDs) to evaluate potential disease transmission to contacts and human exposures.
- Educating and conducting outreach activities with community partners and other stakeholders on zoonotic and vector-borne disease prevention and mitigation.
- Maintaining response plans to ensure a timely and effective response in the event of the emergence of a zoonotic and/or vector-borne disease in the community.
Communicable Diseases and Outbreak Management
- Preventing and reducing the spread of infectious and communicable diseases recognized as Diseases of Public Health Significance (DoPHS).
- Conducting case and contact investigations upon receiving reports from primary health care providers, labs, schools, childcare settings, and congregate living settings.
- Reporting on and reviewing surveillance data to identify trends, outbreaks, and clusters to inform response decisions.
- Recognizing emergent infections.
- Strengthening knowledge of infection prevention and control (IPAC) practices, the Mandatory Blood Testing Act (MBTA), and procedures for managing exposures to bloodborne pathogens to Emergency Service Workers (ESW).
- Managing applications and inquiries for Mandatory Blood Testing Act.
- Enhancement of IPAC knowledge and preparedness in licensed childcare settings.
- Investigating and managing all reports of suspected or confirmed infectious disease outbreaks and clusters and declaring outbreaks.
- Collaborating with public health inspectors who conduct site visits, validating internal facility policies, and ensuring the implementation of IPAC measures.
IPAC Hub
- Supporting congregate living settings through tailored, on-site, and remote IPAC guidance.
- Providing congregate living settings with mentorship and expertise in the development of customized IPAC and outbreak programs, policies, and management plans.
- Evaluating the current IPAC practices, identifying gaps, and guiding quality improvement efforts in target, high-risk congregate living settings.
- Hosting community information sessions to foster peer-to-peer learning.
Sexually Transmitted and Blood-Borne Infections (STBBI)
- Investigating and managing all reported cases of STBBIs to minimize the spread of infection through case and contact management.
- Identifying and implementing outreach strategies to increase knowledge and awareness of STBBIs among healthcare providers and partners.
- Engaging healthcare providers to build capacity for STBBI services and care and implementing strategies focusing on increasing knowledge of STBBI treatment and testing.
- Supporting priority and high-risk populations to promote healthy sexual practices and increase access to sexual health services.
- Dispensing publicly funded medications and vaccines to community partner organizations.
Tuberculosis
- Investigating and managing TB medical surveillance referrals, suspected or confirmed active TB disease, contacts of TB disease, and individuals with latent TB infection.
- Dispensing preventive treatment to clients and community partners at no cost.
- Implementing community outreach initiatives to increase awareness of TB screening and preventive treatment in high-risk populations.
Safe Water
Under the Safe Water standard, boards of health are required to prevent or reduce illnesses and health hazards related to drinking water and recreational water use.
In 2024, there were 158 recreational water facilities operating in Windsor and Essex County, including public pools, wading pools, splash pads, and spas. WECHU Public Health Inspectors conducted inspections of these facilities, responded to 11 complaints, and issued five closure orders (Section 13) to address identified health hazards.
In 2025, seven public beaches were tested weekly for E. coli levels and blue-green algae over a 14-week monitoring period. A total of 25 water-quality warnings (201–999 E. coli/100 mL) and five closures (≥1,000 E. coli/100 mL) were issued.
The region’s 14 municipal water treatment and distribution systems provide most residents with safe drinking water, supported by continuous monitoring and corrective actions for any adverse water quality incidents (AWQIs). In 2024, 16 AWQIs were reported and investigated, leading to 15 boil water advisories (BWAs), one of which required public notification through media channels due to its scope of impact.
Small Drinking Water Systems (SDWS), particularly those on Pelee Island, continue to receive inspections and risk assessments. Of the 35 SDWS in operation (34 on Pelee Island), 10 inspections were completed in 2024. During this time, 11 AWQIs were reported and addressed within 24 hours, resulting in eight boil water orders due to bacterial or microbiological contamination.
In 2024, there were 25 confirmed cases of giardiasis (4.9 per 100,000). From January to July 2025, eight cases have been reported. Additional 2024 cases included six hepatitis A and one cyclosporiasis infection, with two hepatitis A and one cyclosporiasis case reported between January and June 2025.
Below is a list of the program(s) under the Safe Water standard along with examples of work included under each:
Safe Water
- Conducting surveillance and inspection of all recreational water premises within its jurisdiction and disclosing results of routine and complaint-based inspections.
- Monitoring water testing results and recommending corrective action when notified of any adverse water quality incidents, including those from local school boards and municipalities.
- Ensuring 24/7 on-call response to suspected waterborne illness or outbreaks, complaints, and adverse results and observations.
- Routine and re-inspections, risk assessments and education for owners and operators of Small Drinking Water Systems (SDWS), particularly on Pelee Island.
- Conducting the beach monitoring program including predictive modelling program during the summer season for E. coli and blue-green algae blooms, issuing advisories when needed, and collaborating with local municipalities to ensure water safety at beaches.
Substance Use Prevention & Harm Reduction
The goal of the Substance Use Prevention standard is to prevent and reduce harms associated with substance use and promote protective factors that support health and well-being.
Local data highlight ongoing challenges related to opioids, alcohol, cannabis, and other substances. Opioid-related emergency department (ED) visits in WEC have risen sharply, increasing from 10.1 per 100,000 population in 2015 to 95.93 per 100,000 in 2024. Rates have exceeded provincial averages in most years since 2015. Opioid-related deaths have also increased, from 5.9 per 100,000 in 2015 to 19.7 per 100,000 in 2024, peaking at 28.9 per 100,000 in 2023, a rate consistently above the provincial average. Cocaine-related ED visits remain higher than the provincial rate, with 90.75 visits per 100,000 population in WEC compared to 77.96 provincially in 2024.
Alcohol use continues to be the leading cause of substance-related ED visits in WEC. In 2024, there were 2,059 alcohol-attributable ED visits, and the hospitalization rate (271.78 per 100,000) exceeded the provincial rate (192.77 per 100,000).
According to the Canadian Community Health Survey (2020), 14.2% of WEC adults reported smoking occasionally or regularly, higher than the provincial rate of 12.4%. Smoking was most prevalent among 45–64-year-olds and individuals with lower income or education. Among youth, the Ontario Student Drug Use and Health Survey (2023) found that 17.2% of students in grades 7–12 had tried vaping, with 5.6% reporting daily use.
Below is a list of the program(s) under the Substance Use and Injury Prevention standard along with examples of work included under each:
Local/Provincial Regulatory Compliance and Enforcement
- Enforcing the Smoke-Free Ontario Act, 2017 (SFOA) to reduce youth access to tobacco and vapour products and minimize exposure to second-hand smoke and vapour.
- Conducting mandatory inspections at tobacco and vapour product retail locations to ensure compliance with display, promotion, and handling regulations, and inspecting specialty vape stores prior to operation.
- Carrying out proactive compliance inspections at high-risk locations (e.g. restaurants/bars, festivals, and outdoor smoke-free areas such as playgrounds and sports fields)
- Supporting municipal partners through policy consultation, by-law review, and guidance on emerging tobacco and vapour-related issues.
Reducing Substance-related Harms
- Providing harm reduction resources, supplies, education, services, and training to people who use drugs and those who support them, with a focus on preventing overdose, injury, and death.
- Delivering education and tools to promote safer consumption, overdose prevention, and emergency response.
- Coordinating partnerships across community organizations, institutions, and people with lived and living experience to drive policy and community-based solutions that reduce substance-related harms.
- Building healthy public policy related to substance use and enhancing data-sharing and transparency among agencies and the public.
- Using population health data, community health assessments, and structured engagement with people with lived/living experience to inform interventions that reduce health and social disparities.
Substance Use Prevention and Supports
- Creating and maintaining physical, social, built, and economic environments that support substance use prevention, harm reduction, and access to treatment services.
- Coordinating the local implementation of the Icelandic Prevention Model (IPM) through coalition-building, stakeholder engagement, youth surveys, and data analysis to guide community-specific prevention strategies.
- Creating and enhancing supportive environments across various community settings to support substance use prevention, treatment, and harm reduction in Windsor-Essex County.
- Implementing structural and educational supports to reduce barriers to services and minimize substance-related harms among priority populations, including enhanced system navigation.
- Collaborating with local community partners to create supportive environment approaches in the areas of youth substance use prevention and treatment access for priority populations.
- Providing education on safe handling and disposal of medications.
- Support system navigation through WEC Connect, an online inventory of substance use, mental health, and behavioural addiction services.
